The Maryland Clean Collaborative: Successfully Tackling HAI Prevention
About the Author: Shari L. Solomon, Esq. currently serves as a Board of Director for the Healthcare Surfaces Institute. Solomon, an attorney by trade, works to provide infection prevention and industrial hygiene training and consulting services geared toward healthcare personnel responsible for infection prevention, cleaning and disinfection, and facility operations and maintenance practices. She is president of CleanHealth Environmental, LLC, a Designated Trainer under the Certified Healthcare Environmental Services Technician Program (T-CHEST) from The Association for the Healthcare Environment (AHE) of the American Hospital Association. For more information, check out her Linked In profile and her professional website cleanhealthenv.com.
It is well recognized that healthcare-associated infections (HAIs) are a major threat to patient safety.
According to the Center for Disease Control and Prevention (CDC), each year, about 1 in 25 U.S. hospital patients are diagnosed with at least one infection related to hospital care alone; additional infections occur in other healthcare settings. Despite healthcare facility efforts to reduce HAIs caused by pathogens including Clostridium difficle (CDI), methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), Acinetobacter baumani, and carbapenem-resistant Enterobactereciae (CRE), they continue to plague healthcare facilities and their patients.
Over the past decade, research studies have found sufficient evidence that cleaning and disinfecting environmental surfaces in healthcare facilities is fundamental in reducing the incidence of healthcare-associated infections. Contaminated environmental surfaces, contaminated equipment, and contaminated hands of healthcare workers have all been linked to the transmission of several pathogens, which have led to individual cases and multiple outbreaks of healthcare-associated infection[1]. Healthcare personnel come in contact with environmental surfaces frequently in patient’s rooms and other public areas. These frequently touched surfaces may serve as a reservoir for these infectious pathogens as they can survive on inanimate surfaces for prolonged periods. For example, organisms such as MRSA and VRE have been shown to persist on dry surfaces for several weeks to months[2]’[3]’[4]. In response, the CDC recommends that hospitals optimize the thoroughness of their high-touch surface cleaning and use a validation monitoring system to ensure that facilities are being cleaned.
The Clean Collaborative Framework
Recognizing these challenges, the state of Maryland created a cutting-edge program, called The Clean Collaborative (The Collaborative), to tackle a key component of these infection transfers – surface contamination. The first of its scale in the United States, Program Director CleanHealth Environmental, partnered with the Maryland Patient Safety Center, to launch this statewide program. Utilizing CDC recommendations on high-touch surface cleaning, the Clean Collaborative highlights the need for facilities to address cleaning and validation monitoring, as well as to facilitate collaboration among healthcare facilities by providing shared data, best practices and emerging technologies to tackle HAIs.
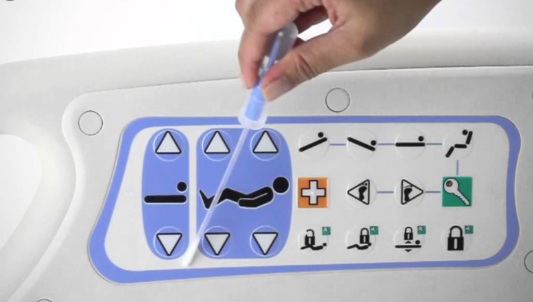
The Collaborative supported 17 acute care hospitals, three long-term care facilities, and four ambulatory surgical centers throughout Maryland, in improving environmental surface cleaning. Cleaning effectiveness was quantified using Hygiena’s ATP monitoring validation technology, measured in relative light units (RLUs), which serves as an indicator of the bioburden remaining on a surface. The Clean Collaborative team identified specific sampling locations in the patient rooms and public areas using the CDC Environmental Checklist. Acute care hospitals and long-term care facilities collected 100 swabs per month and ambulatory surgical centers collected 25 swabs per month. These sampling locations stemmed from CDC’s recommended high touch surfaces, as well as other high touch surface areas identified to harbor infectious pathogens. Participants collected and reported data for 12 months (April 2016 – March 2017) and inputted the data in a shared web-based portal. Participants also received training on the use of ATP technology, webinars on topics such as surface cleaning, surface disinfection and product selection, and fact sheets highlighting cleaning and disinfection best practices.
A primary goal of The Collaborative was to reduce Clostridium difficile (CDI) infection rates, which the Collaborative team selected as a proxy for HAIs[5],[6],[7]. The CDC estimates that Clostridium difficile (C Diff) infection can cost up to $4.8 billion each year in healthcare cost for acute care facilities alone. C. difficile spores have been shown to survive in the environment for as long as 5 months[8]. Hence, appropriate cleaning and disinfection of these surfaces is an important part of an overall strategy to reduce the risk of healthcare-associated infections (HAIs).
Results of The Clean Collaborative
The results of The Clean Collaborative, published in the American Journal of Infection Control, were impressive. Twenty-one (21) of the 24 participating facilities (88%) achieved the goal of a 10% reduction in RLUs from the baseline month to the final month of the Collaborative. Seventy-five percent of participating facilities exceeded this goal by reducing average RLUs by more than 50%.
The Collaborative team also compared the CDI rates of participating facilities with the CDI rates of non-participating facilities in Maryland. A 14.2% decrease in CDI rates compared to only a 5.9% decrease among non-participating facilities was observed from the baseline month to the final month.
In addition to these positive quantitative outcomes, this initiative has proved effective in fostering collaboration and implementing best practices between healthcare professionals. The Collaborative was a success and created a platform for infection preventionists, environmental services and other healthcare professionals to work as a team in achieving a shared goal. For example, environmental services teams partnered with other departments, such as Security, to require the lobby desk workers to take responsibility for cleaning public surfaces at the beginning of their shift. Infection preventionists also provided immediate feedback to Environmental Services technicians, following swab collection, which encouraged enhanced cleaning processes in a timely manner. Furthermore, based on the feedback of swab collection results, participating facilities were able to implement additional internal measures including the use of engineering controls such as automatic doors, automatic flushers and hand sanitizers to enhance cleaning results.
The Clean Collaborative Model Can be Replicated
Multiple studies have demonstrated that less than 50% of hospital room surfaces are adequately cleaned and disinfected[9],[10]. Interventions, including improved education of environmental services workers, checklists to assure that all surfaces (usually by environmental service workers) and medical devices/equipment (usually by nursing) are cleaned and disinfected, and validation of the cleanliness of the environment (e.g., fluorescent dye, ATP), including immediate feedback to the environmental services worker, have been demonstrated to improve the frequency of adequate cleaning in the range of 71–77%6,7.
The framework of The Collaborative has been successfully applied to other healthcare systems and can be replicated in similar statewide programs and healthcare systems, with the goal of improving cleaning and disinfection practices and reducing HAIs. This can be achieved through validation technology to measure cleaning effectiveness, education in cleaning and disinfection, and tracking monthly quantitative data to modify internal procedures.
Phase II of The Collaborative, which focuses on building upon the lessons learned during Phase 1, is already underway. Phase II continues the focus on high-touch surface areas in patient rooms as well as additional locations of concerns including the emergency departments, nursing stations and durable medical equipment.

Shari Solomon is an integral and unique Board of Director for the Healthcare Surfaces Institute, bringing both healthcare and legal perspectives to the mission: To reduce preventable infections through collaboration of industry, academia, science, regulatory, and service sectors by interrupting the transmission of surface-related pathogens in healthcare in support of community health.
Our organization supports her professional expertise as it brings healthcare surfaces to the forefront of the battle against HAIs.
References:
[1] Huslage K, Rutala WA, Sickbert-Bennett E and Weber DJ. A Quantitative Approach to Defining High-Touch Surfaces in Hospitals. Infection Control and Hospital Epidemiology, Vol. 31, No. 8 (August 2010), pp. 850-853.
[2] Wagenvoort JH, Sluijsmans W, Penders RJ. Better environmental survival of outbreak vs. sporadic MRSA isolates. Journal of Hospital Infection. 2000 Jul;45(3):231–4.
[3] Wendt C, Wiesenthal B, Dietz E, et al. Survival of vancomycin-resistant and vancomycin-susceptible enterococci on dry surfaces. Journal of Clinical Microbiology. 1998 Dec;36(12):3734–6.
[4] Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infectious Diseases. 2006 Aug 16
[5] Zimlichman, E., Henderson, D., Tamir, O., Franz, C., Song, P., Yamin, C. K., . . . Bates, D. W. (2013). Health Care–Associated Infections. JAMA Internal Medicine,173(22), 2039. doi:10.1001/jamainternmed.2013.9763
[6] Weber, D. J., Rutala, W. A., Miller, M. B., Huslage, K., & Sickbert-Bennett, E. (2010). Role of hospital surfaces in the transmission of emerging health care-associated pathogens: Norovirus, Clostridium difficile, and Acinetobacter species. American Journal of Infection Control, 38(5). doi: 10.1016/j.ajic.2010.04.196
[7] Weinstein, R. A., & Hota, B. (2004). Contamination, Disinfection, and Cross-Colonization: Are Hospital Surfaces Reservoirs for Nosocomial Infection? Clinical Infectious Diseases, 39(8), 1182-1189. doi:10.1086/424667
[8] Kim KH, Fekety R, Batts DH, et al. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. Journal of Infectious Disease. 1981 Jan;143(1):42–50.
[9] Carling PC, Parry F, von Beheren M. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infection Control & Hospital Epidemiology. 2008; 29:1–7.
[10] Goodman ER, Platt R, Bass R, et al. Impact of environmental cleaning intervention on the presence of methicillin-resistant Stahylococcus aureus and vancomycin-resistant enterococci on surfaces in intensive care unit rooms. Infection Control & Hospital Epidemiology. 2008; 29:593–599.